Most therapists spend months building CBT skills with clients, then allocate only 10 minutes for discharge planning.
The result? Clients who can challenge thoughts beautifully in session but fall apart at 2am, facing their first panic attack alone.
This happens more often than it should. Sometimes clients announce unexpectedly that next session will be their last. Sometimes fixed session limits mean you’re still addressing core issues when time runs out. But honestly, therapist training rarely covers discharge planning well.
Table of Contents
There’s a skill gap here. Research shows that structured discharge planning significantly decreases relapse rates.
Plan Independence From Session One
The first thing to change about your final sessions? Stop thinking about them as final sessions.
Start planning discharge from session one.
Get your client to recognise that becoming their own therapist is one of the key aims of CBT overall. They’re building a new repertoire of skills, perspectives, and a practical toolkit to draw on when needed.
This isn’t about dependency. It’s about genuine autonomy.
However, there’s a significant difference between a client who can utilise CBT skills with your guidance and one who can effectively be their own therapist during a crisis. You need them to really understand the techniques.
For panic attacks, that means breathing management, mindfulness, and challenging catastrophic thoughts. Help them practice these skills in session and in the real world. Ensure they’re ready to utilise their skills when needed.
The key principle is to avoid discharging too early. Clients need to prioritise self-management first.
The Case Study Assessment Technique
How do you actually assess if someone has moved from knowing techniques to being ready for independence?
First, ask directly if they feel ready for discharge. Frame it as “how many more weeks?” rather than “shall we make this the last session?”
But here’s a specific technique that reveals true readiness: use case studies.
Give your client a case study similar to theirs. Say something like: “If you were Tom’s therapist, what advice would you give him? What would you encourage him to think about regarding his behaviour or perspectives?”
This is brilliant because you’re getting them to step into the therapist role without the pressure of it being about themselves.
This isn’t a test. It’s the start of a conversation where you both identify what areas need revisiting, rehearsing, or strengthening.
Ready clients suggest multiple intervention options for Tom. They recognise challenges and suggest what to do if something doesn’t work as planned.
Clients who need more time give single solutions or miss obvious complications.
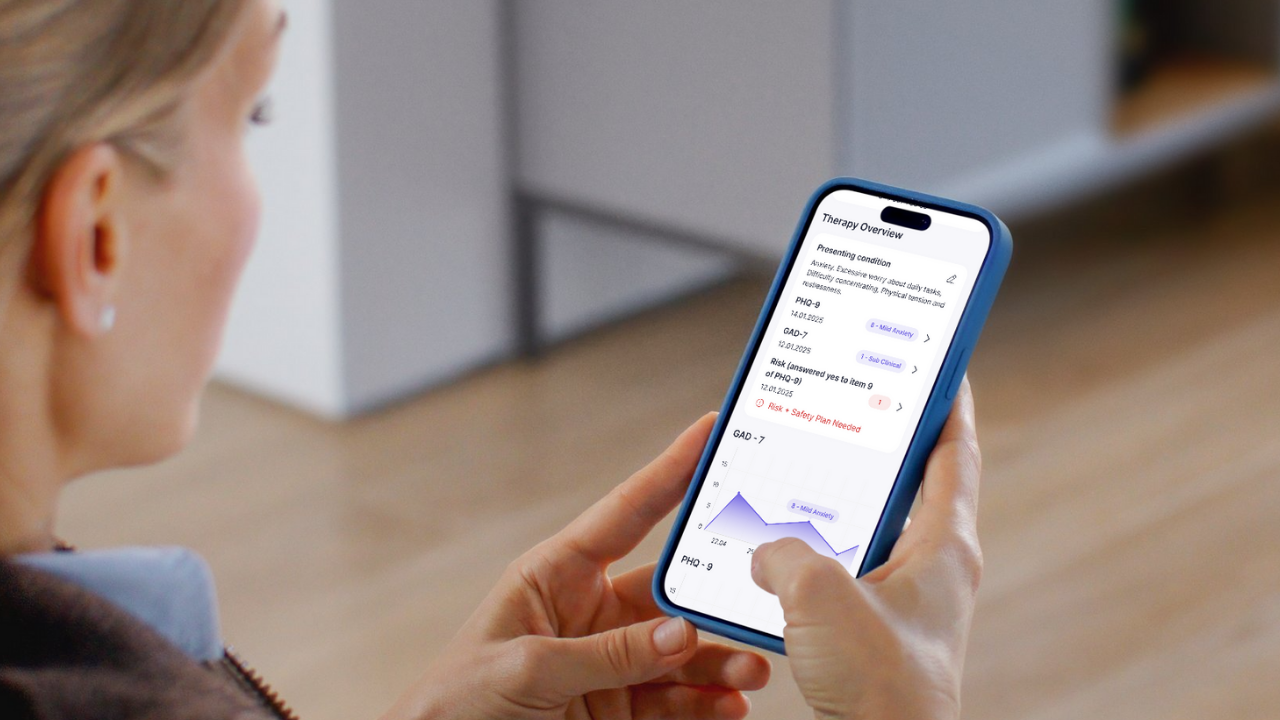
Of course, monitor symptoms throughout. Any risk issues need to be front and center of discharge decisions.
Build Future-Focused Resilience
Help clients consider potential future threats to relapse. Anniversaries, family gatherings, and periods of work stress.
But alongside identifying triggers, help them map their social support network. Who can they call? What resources do they have?
This needs to be incorporated from the first session, with skill sets monitored throughout. Digital platforms like Flutura can support this monitoring process, tracking progress and engagement during those crucial 167 hours between sessions.
Digital Tools That Actually Work
There’s often a disconnect between what works in digital tools and what clients actually use when struggling.
The key is to ensure that clients view the app as supporting face-to-face sessions, not replacing them.
Balance therapist-assigned tasks with client-initiated activities based on their mood or challenges. Let them build confidence in choosing their own interventions.
But be clear about boundaries. In severe crisis moments, calling emergency services or specialist support lines remains Plan A.
The Gradual Transition Process
The transition from client to self-therapist isn’t a sudden quantum leap overnight.
It’s a gradual, collaborative process that culminates in genuine confidence, allowing you to use a range of tools independently.
In those final sessions, you’re doing something different. You’re not just processing current issues or reviewing progress.
You’re rehearsing independence. Walking through scenarios. Testing their decision-making about which tools to use when.
You’re building their confidence in trusting their own judgment about when to use breathing techniques, when to challenge their thoughts, and when to seek support.
Making It Practical
Start your next session differently. Instead of diving into current concerns, spend five minutes discussing what independence will look like for this specific client.
What will their toolkit contain? How will they know when to use which technique?
Try the case study technique in your next appropriate session. Create a scenario similar to your client’s situation and see how they respond as the “therapist.”
You can use their response to guide your remaining sessions. What gaps emerged? What strengths can you build on?
The goal isn’t perfect self-management. It’s confident, flexible problem-solving when challenges arise.
Because at 2am during a panic attack, your client won’t remember everything from therapy. But they’ll remember the process of working through problems systematically.
That’s what transforms CBT techniques into lasting life skills.
Plan for that transformation from session one, assess it thoughtfully, and support it with the right tools. Your clients will thank you for preparing them not just for the end of therapy, but for the beginning of their independence.