Depression can make even the simplest tasks feel overwhelming, including therapy homework. When you’re working with clients who struggle to get out of bed, asking them to complete thought records or behavioural experiments can feel like asking them to climb a mountain.
You know CBT works, but you also know that its task-based approach can overwhelm clients when their motivation is at rock bottom.
This guide provides practical guidance on using digital tools compassionately. We’re not talking about apps that nag or pressure your clients. Instead, you’ll learn how technology can gently support them between sessions, making CBT feel more manageable when everything else feels impossible.
Table of Contents
What Makes CBT Hard for Clients with Depression
Depression creates unique challenges that can make CBT feel like climbing a mountain with weights tied to your ankles. Understanding these barriers helps us support clients more effectively.
Low energy and motivation affecting task completion
Depression drains energy like nothing else. Simple tasks become monumental efforts. When a client can barely get out of bed, completing thought records or behavioural experiments feels impossible. This isn’t laziness—it’s a core symptom that directly conflicts with CBT’s active approach 1.
Cognitive symptoms making it difficult to remember or organise between-session work
Depression affects concentration, memory, and decision-making. Clients might forget what they discussed in therapy or struggle to organise homework tasks. They may read the same worksheet three times without absorbing it. These cognitive symptoms create a frustrating cycle where clients want to engage but literally can’t think clearly enough to do so.
Shame spirals when clients can’t complete homework
When depression already whispers “you’re worthless,” incomplete homework becomes “proof” of failure. Clients may avoid sessions rather than admit they haven’t done their tasks. This shame creates distance in the therapeutic relationship precisely when connection matters most. The very structure meant to help becomes another source of self-criticism.
Avoidance patterns that strengthen when tasks feel too demanding
Depression and avoidance go hand in hand. When CBT tasks feel overwhelming, clients naturally pull back. This avoidance provides short-term relief but strengthens depression’s grip long-term 2. Each avoided task makes the next one feel even harder, creating a downward spiral that’s difficult to break.
Why Traditional Approaches Often Fall Short
Paper worksheets pile up in bags, forgotten until the next session. Generic email reminders land in inboxes already full of demands. Standard homework sheets feel like school assignments when clients are already struggling to shower or eat.
These traditional tools weren’t designed for depression’s reality. They assume motivation that isn’t there. They expect organisation skills that depression steals. Most importantly, they miss the shame that builds when clients can’t complete “simple” tasks.
One-size-fits-all homework creates pressure, not progress. When every client gets the same thought record or activity schedule, it ignores their unique struggles. A working parent with depression needs different support than a university student. Yet traditional CBT materials rarely adapt.
Progress becomes invisible through depression’s lens. Clients genuinely can’t see their improvements. They forget the good days. They dismiss small wins. Paper records get lost or avoided, making it impossible to show concrete evidence of change when clients need it most.
Administrative tasks steal precious session time. You’re reviewing homework, chasing missing forms, explaining tasks again. Meanwhile, the therapeutic relationship—your most powerful tool—gets squeezed into smaller windows. Clients sense the rush and feel like another task on your list.
The result? Disconnection grows. Clients feel they’re failing at therapy. You feel you’re not reaching them. The very tools meant to help become barriers to healing. This cycle strengthens depression’s voice that says “nothing works” and “I can’t do anything right.”
Digital tools designed for therapy can break this pattern. But only if they’re built with genuine understanding of depression and the therapeutic relationship. The next sections will show you how.
What You’ll Need Before Adding Tech to Your Practice
Before introducing digital tools into your CBT practice, you’ll need more than just the right software. Success depends on thoughtful preparation and a client-centred approach.
Clear understanding of your client’s relationship with technology. Start by exploring how comfortable your client feels with digital tools. Some clients find apps empowering, whilst others feel overwhelmed by another thing to manage. Ask about their current tech use, any past experiences with mental health apps, and what devices they prefer.
Consent and collaboration around digital tool use. Never introduce technology without explicit consent and genuine collaboration. Explain exactly how digital tools will support their therapy, what data will be collected, and how it will be used. Make it clear that using tech is optional and won’t affect the quality of care they receive 3.
Platform that respects clinical boundaries and privacy. Choose tools that comply with privacy regulations and protect client data. Look for platforms designed specifically for therapy rather than general wellness apps. Ensure the technology maintains appropriate therapeutic boundaries and doesn’t blur professional relationships 3.
Flexibility to adjust based on client feedback. Be prepared to modify or discontinue tech use if it’s not helping. Build in regular check-ins about how the tools are working. Some clients might need simpler features, whilst others benefit from more detailed tracking. Your willingness to adapt shows that the therapeutic relationship comes first, not the technology.
Building a Compassionate Digital Framework
Start with collaborative goal-setting
- Involve clients in choosing their level of digital interaction
- Set realistic expectations together
- Build in permission to pause or adjust
Choose tools that support autonomy
- Opt-in features rather than defaults
- Client-controlled privacy settings
- Flexibility in timing and frequency
Focus on connection, not compliance
- Frame tools as support, not surveillance
- Emphasise progress over perfection
- Maintain human touch points
Common Mistakes to Avoid
- Defaulting to “more reminders” when engagement drops
When clients aren’t responding, adding more notifications often backfires. Depression already brings guilt and overwhelm. Extra reminders can feel like nagging, pushing clients further into avoidance. - Using generic, impersonal messaging
“Don’t forget your homework!” feels cold and demanding. Messages need warmth and flexibility. Consider “When you’re ready, your thought record is here” instead. Small wording changes make a big difference. - Forcing gamification or productivity framing
Points, streaks, and leaderboards work for some. But competitive elements can increase pressure for depressed clients. They need compassion, not competition. Let clients choose whether they want these features. - Replacing human support with automation
Tech should enhance your relationship, not replace it. Automated messages can’t read context or offer genuine empathy. Keep the human connection central, using tools to support (not substitute) your therapeutic presence. - Ignoring signs that tech is increasing pressure
Watch for increased shame, avoidance, or session cancellations after introducing digital tools. If a client starts apologising for “failing” the app, it’s time to reassess. Tech should reduce burden, not add to it.
Personalising for Each Client
Assessment questions to ask before introducing tools
Start by exploring your client’s current relationship with technology. Ask about their daily tech use and comfort level. Find out if they’ve tried mental health apps before and what worked or didn’t. Check whether notifications feel supportive or stressful to them. Understanding their baseline helps you match tools to their needs, not yours.
Red flags that suggest tech might not help
Watch for signs that digital tools might add pressure. If a client expresses feeling overwhelmed by their phone already, pause. Notice if they mention past experiences of app-related guilt or shame. Be cautious when perfectionism runs high. Some clients might turn helpful tools into another source of self-criticism. Tech fatigue is real, especially for those juggling multiple digital demands.
Adjustment strategies when initial approaches don’t work
When engagement drops, resist adding more features. Instead, simplify. Reduce reminder frequency or switch to weekly rather than daily check-ins. Let clients choose their preferred communication style, some prefer brief texts whilst others need visual prompts. Consider seasonal adjustments too. Depression often worsens in winter, so lighten the digital load during harder months.
Success indicators beyond task completion
Look for quality of engagement over quantity. A client who completes one meaningful mood entry beats one who rushes through daily tasks. Notice if they’re sharing more openly in sessions about their between-session experiences. Watch for increased self-compassion in how they discuss incomplete tasks. Success might look like a client saying “I only managed half, but that’s okay” rather than giving up entirely.
What Success Really Looks Like
Success isn’t about perfect homework completion or daily mood logs. It’s about creating a supportive digital environment that helps clients engage with therapy on their terms.
Clients feeling supported, not surveilled
Watch for signs that clients see digital tools as helpful companions rather than watchful eyes. They’ll start sharing more openly about their struggles with tasks. They’ll tell you when something isn’t working instead of pretending everything’s fine.
Increased session engagement and openness
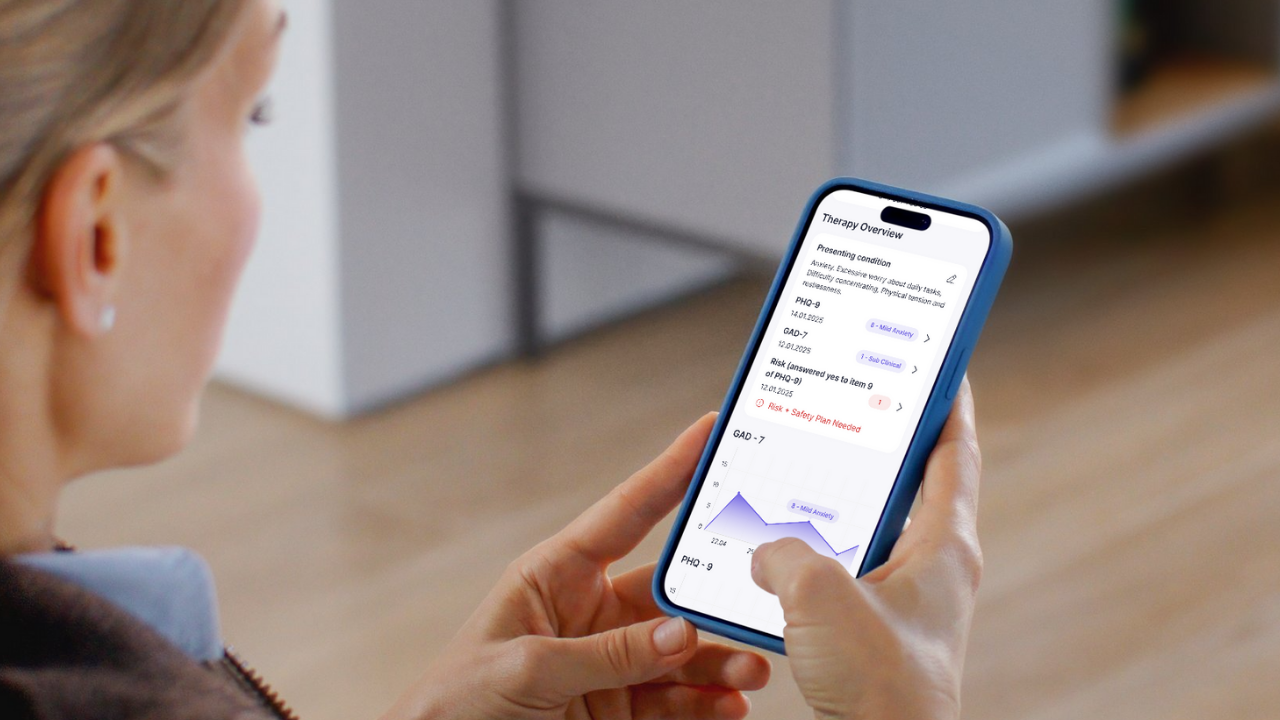
When digital tools work well, clients arrive at sessions with more to discuss. They’ve noticed patterns in their mood tracking. They want to explore why certain days felt harder. The tools become conversation starters, not report cards.
Gradual improvement in between-session follow-through
Progress might start small, a client who checks in once a week instead of never. Someone who completes one thought record instead of giving up entirely. These tiny wins matter more than perfect adherence.
Stronger therapeutic alliance despite (or because of) digital elements
The right tools actually strengthen your relationship. Clients feel you understand their daily struggles. They appreciate the flexibility and compassion built into the system. Technology becomes a bridge, not a barrier.
Reduced therapist admin time without sacrificing care quality
You’ll spend less time chasing updates and more time providing therapy. Automated check-ins give you insights before sessions start. Progress tracking happens without manual data entry. This efficiency creates space for deeper therapeutic work.
Remember: success looks different for each client. Some might embrace every feature whilst others use just one or two tools. Both approaches are valid when they support genuine therapeutic progress.
Next Steps for Your Practice
- Start small with one willing client who’s open to trying digital support. Choose someone who already uses technology comfortably and has expressed frustration with traditional homework methods. This lets you test the waters without overwhelming yourself or your client.
- Track both clinical outcomes and client feedback throughout the process. Note changes in homework completion, session engagement, and therapeutic alliance. More importantly, ask clients directly how the tools feel. Are they helpful or adding pressure?
- Adjust your approach based on what you learn. If reminders feel pushy, try weekly check-ins instead. If mood tracking becomes obsessive, switch to simple rating scales. Remember, the goal is support, not perfection.
- Share insights with colleagues to build best practices. Many therapists face similar challenges with depressed clients. Your experiences (both successes and setbacks) can help others navigate digital tools more effectively.
- Consider purpose-built tools designed for therapeutic use. Generic productivity apps often miss the mark for clinical work. Look for platforms created with therapist input that understand the nuances of depression treatment.
Help Your Clients Thrive with the Right Tech
If you’re ready to support your depressed clients with technology that truly understands CBT, we’re here to help. Flutura was built by therapists who know that depression requires compassion, not just clever features.
Join our waitlist to be first to explore tools designed specifically for your practice. You’ll get access to free resources while you wait, including templates for gentle task reminders and progress tracking guides.
Join the Flutura waitlist today and discover how the right tech can strengthen (not strain) your therapeutic relationships.
References
- Behavioural Activation Depression – https://medicine.umich.edu/sites/default/files/content/downloads/Behavioral-Activation-for-Depression.pdf[↑]
- Predictors of engagement with between-session work in Cognitive Behavioural Therapy (CBT)-based interventions – https://www.tandfonline.com/doi/full/10.1080/16506073.2024.2369939[↑]
- Ethical Use of Artificial intelligence in Counseling Practice
– https://www.nbcc.org/resources/nccs/newsletter/ethical-use-of-ai-in-counseling-practice[↑][↑]